Reflections from the Joint Learning Exchange Forum
By Health Procurement Africa, inSupply Health, Africa Resource Centre, and ThinkWell
On August 28, 2025, health supply chain leaders, government representatives, implementing and development partners, and practitioners gathered in Nairobi for the Health Supply Chain Learning Exchange Forum. What unfolded was not just another meeting but a candid, solution-driven dialogue that underscored both the urgency and opportunity before Kenya: transitioning to a country-led, sustainable health supply chain
The Financing and Supply Chain Challenge
Financing for Health Products and Technologies (HPT) remains a persistent challenge, with delayed exchequer disbursements slowing procurement and affecting product availability at the service delivery points. Counties are tapping into Facility Improvement Funds and exploring innovative options such as pooled procurement and local manufacturing, yet supply chain inefficiencies continue to undermine progress. These inefficiencies are not merely technical; they represent missed opportunities to save lives.
Speaking at the forum, Dr. Ouma Oluga, Principal Secretary for Medical Services – Ministry of Health, reminded participants that health supply chains are the lifeline of service delivery. He urged for solutions that are not only technical, but also patriotic, professional, and pragmatic. Dr. Oluga highlighted persistent breakdowns in facility-level need management, where frontline providers are often excluded from decisions about health facilities’ requirements for HPT, and noted existing skill gaps that hinder accurate forecasting. He also pointed to the rising costs of HPTs, calling for strategies such as local manufacturing, and emphasized the untapped potential of partnerships to strengthen last-mile delivery through multisectoral collaboration.
The Sustainability Imperative
For decades, Kenya’s health system has benefitted from donor investments that kept lifesaving commodities flowing. Yet, as the country strives for universal health coverage and fiscal independence, the question is no longer if sustainability must be achieved, but how fast, and at what cost if delayed.
The Joint Learning Exchange highlighted that declining funding for health supply chain programs is not a distant concern but a pressing reality. Funding gaps are already disrupting programs across Africa and exposing Kenya’s reliance on external support. Counties, in particular, face risks in addressing these gaps, given persistent challenges in reporting, accountability, procurement, and data utilization for informed decision-making. Participants called for a decisive shift: development and implementing partners must move from aid to enablement, aligning investments with Kenya’s UHC agenda, catalyzing scalable innovations, and embedding interventions within national priorities. Reduced donor support also makes local and regional manufacturing an urgent priority, both as a resilience strategy and a pathway to fiscal independence.
Rethinking the Path Forward
Sustainability cannot be achieved by simply replacing donor funds with existing approaches. Instead, Kenya must reimagine how it finances, manages, and delivers HPTs. Forum discussions pointed to new models:
- Financing must expand beyond donor grants to include domestic investment, innovative funding, and public–private partnerships.
- Strategic investments can be made in supply chain design to streamline levels, optimize inventory and expand access through pharmacies for population segments that can pay.
- Workforce optimization is essential, ensuring a skilled, motivated cadre of supply chain professionals.
- Digital tools, once considered add-ons, must now serve as the backbone of accountability, visibility, and efficiency to ensure optimal use of existing resources.
- Markets must be deliberately shaped to strike a balance between affordability, resilience, and equitable access.
- An enabling policy environment is key to strengthening supply chain management across the elements of financing, human resource, procurement and public-private collaborations
County and National Innovations in Action
Counties are increasingly moving beyond routine reporting to actively harness finances, procurement, and quality (F&Q) data for decision-making. This shift is driving measurable improvements in supply chain performance, from more substantial budget allocations and closer monitoring of budget execution, to smarter procurement choices informed by tools such as market price intelligence. With the right people in Health Products and Technologies Units (HPTUs) interpreting and acting on this data, counties are not only improving transparency but also ensuring that resources are aligned with actual needs and service delivery realities.
- Isiolo County reported leveraging quarterly data review meetings to enhance reporting quality and procurement alignment, thereby strengthening its forecasting capacity. This resulted in a 108% increase in budget allocation for FY 2024/25 compared to the previous year.
- Kakamega County demonstrated the value of cross-functional collaboration by utilizing the Strategic Resource Management Tool to enhance prioritization and transparency. As noted by the deputy head of the county HPTU, “We were very pleased with what the tool did. The allocation was based on science and not biased.”
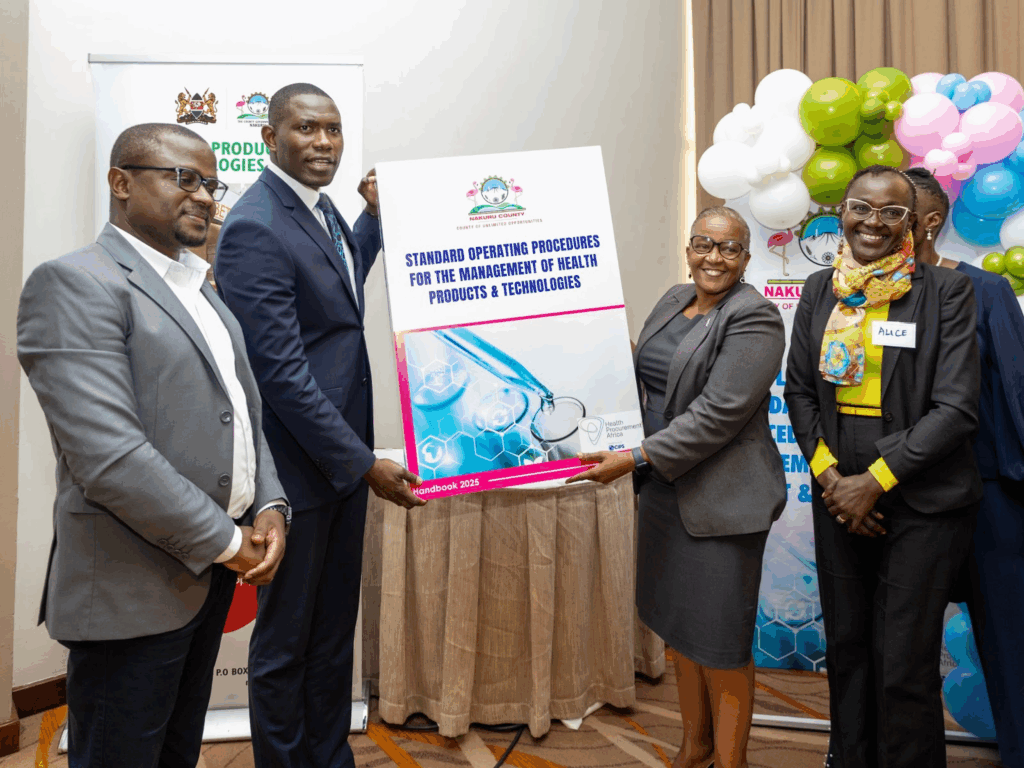
- Nakuru County introduced SOPs and real-time dashboards that enhanced forecasting accuracy, reduced stockouts, and streamlined reporting. As one pharmacist noted, dashboards enabled them to move from “manually mining data” to “interpreting what it means for decisions.”
- Murang’a County advanced automation and e-procurement, raising budget absorption from 56% in 2022 to 98% in 2024 and achieving a 97% fill rate for essential medicines in rural facilities.
National-Level Perspectives
- The Directorate of Health Products and Technologies highlighted that evidence generation to inform policy frameworks remains weak, with many stakeholders struggling to identify policy issues and corresponding actions. Strengthening governance and embedding evidence into decision-making is essential for sustainability.
- The Public Procurement Regulatory Authority (PPRA) guided that counties can leverage economies of scale by establishing joint procuring agencies or engaging in consortium buying to improve HPT availability and affordability.
These experiences underscore that progress is possible, and that local solutions are already reshaping the journey to self-reliance.
Key Takeaways
Governance and Stewardship
- Sustainability requires multi-sectoral collaboration across government, the private sector, and civil society.
- Embedding sustainability goals in national budgets and policies is critical to drive ownership and accountability.
- The National Government must strengthen stewardship through increased domestic financing, transparent policy enforcement, investment in local manufacturing, and digital innovations such as LMIS.
Financing and Resource Management
- Counties must prioritize predictable budgets, timely fund absorption, capacity-building for health workers, and partnerships to ensure last-mile delivery, while the National Government ensures timely disbursement.
- The Facility Improvement Fund has been a game-changer for hospital-level health facilities, as the funds generated are reinvested, supporting HPT availability and enhancing service delivery efficiencies.
Capacity and Resilience
- Local capacity building is urgent; long-term reliance on donor-funded interventions is not a path to resilience.
- Digitalization must be scaled nationwide, not as pilots but as standard practice.
Partnerships and Development Alignment
- Development and implementing partners must align with Kenya’s UHC agenda, shift from aid to enablement, and foster continuous knowledge growth and exchange.
From Dialogue to Action
The Learning Exchange was not an endpoint but a milestone. It reminded all present that the window for action is narrowing, but the path forward is within reach. The real measure of success will not be in eloquent dialogue but in the speed and scale of actions taken.
Kenya’s health supply chain future will be written by the choices made today. The Forum has set the tone; the next step is to match words with actions. This means turning insights into concrete strategies, ensuring that counties and national agencies are better equipped to respond to needs and embedding accountability at every level. It calls for continuous collaboration, not only among policymakers and technical experts, but also with communities who depend on efficient systems for access to essential health products and technologies and services.